We are a BIG deal.
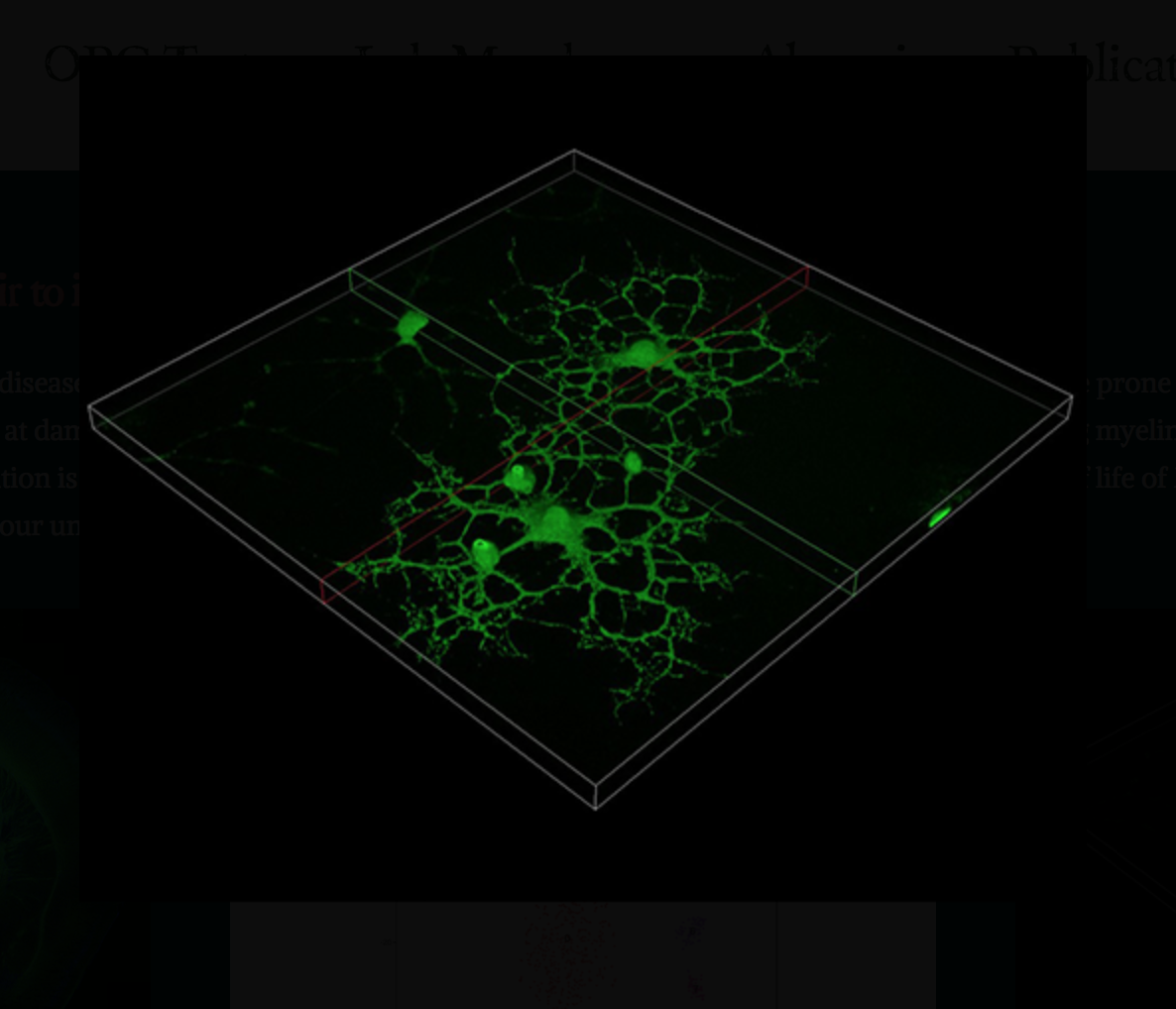
We are a lab within the Center for Brain Immunology and Glia (BIG) at the University of Virginia’s Department of Neuroscience. The lab began with a primary interest in better understanding multiple sclerosis, which is an autoimmune disease that results in damage to the central nervous system, particularly to oligodendrocytes and neurons. Though we continue to look for means to therapeutically target multiple sclerosis, we have also begun to explore other disease models that touch on areas of neuroscience or immunology, as well as their intersection (neuroimmunology).
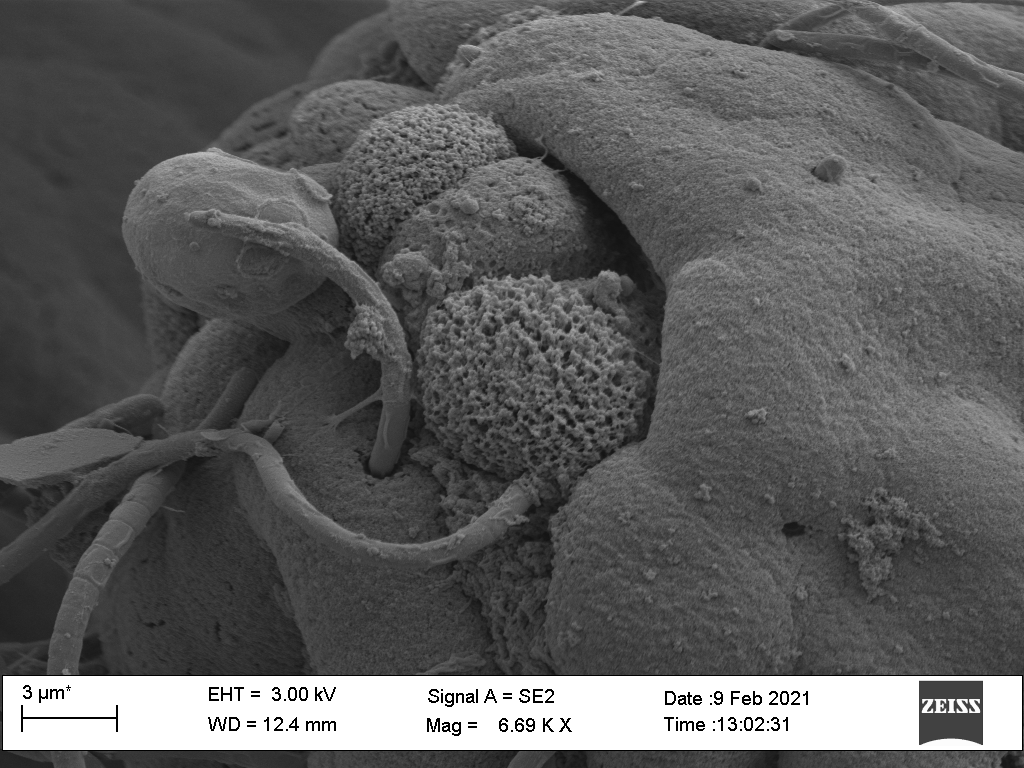
Project #1: Discovering new interventions to tame the immune system during MS.
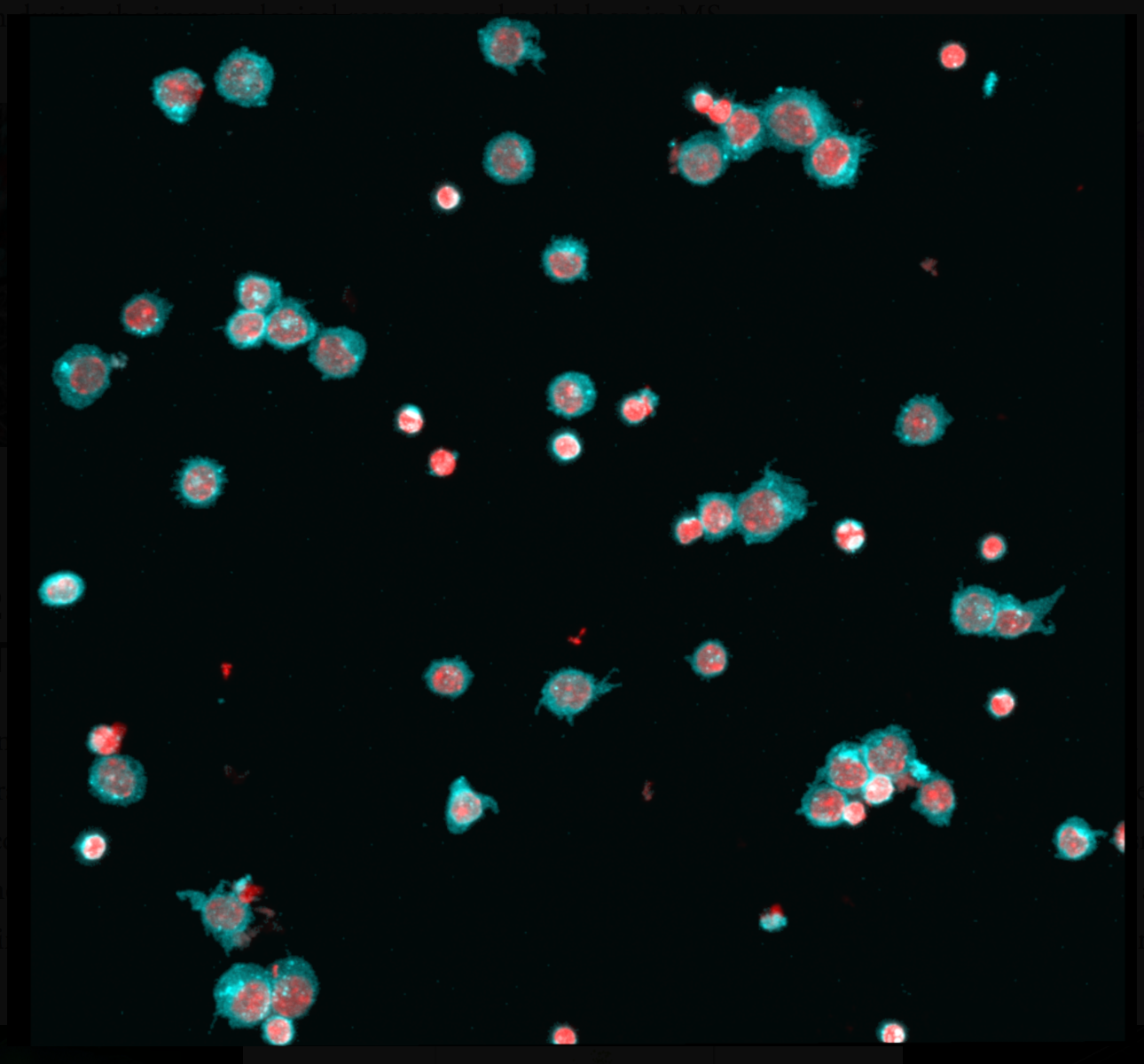
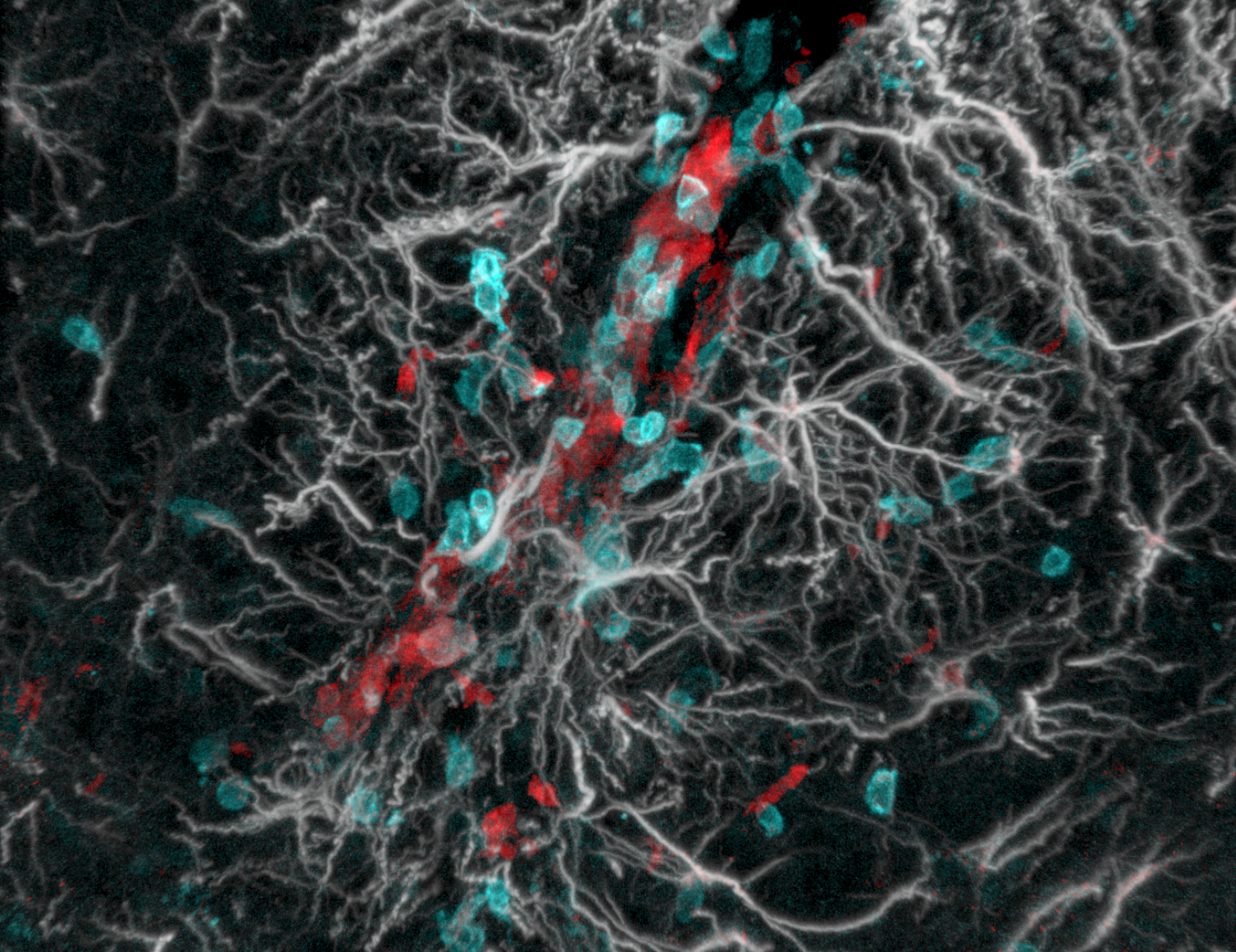
Current immunomodulatory treatments for MS mostly act by blocking the migration of immune cells into the brain. While this strategy is protective, it comes with two major drawbacks; first, the immune-surveillance of the CNS is inhibited, opening the way for opportunistic infections, and second, these therapies are not effective against pathological immune cells that are already “on-site” in the brain. To bypass these pitfalls of first generation therapeutics, we are exploring cellular metabolic states and specific functions of the endoplasmic reticulum during the immunological response and pathology in MS.
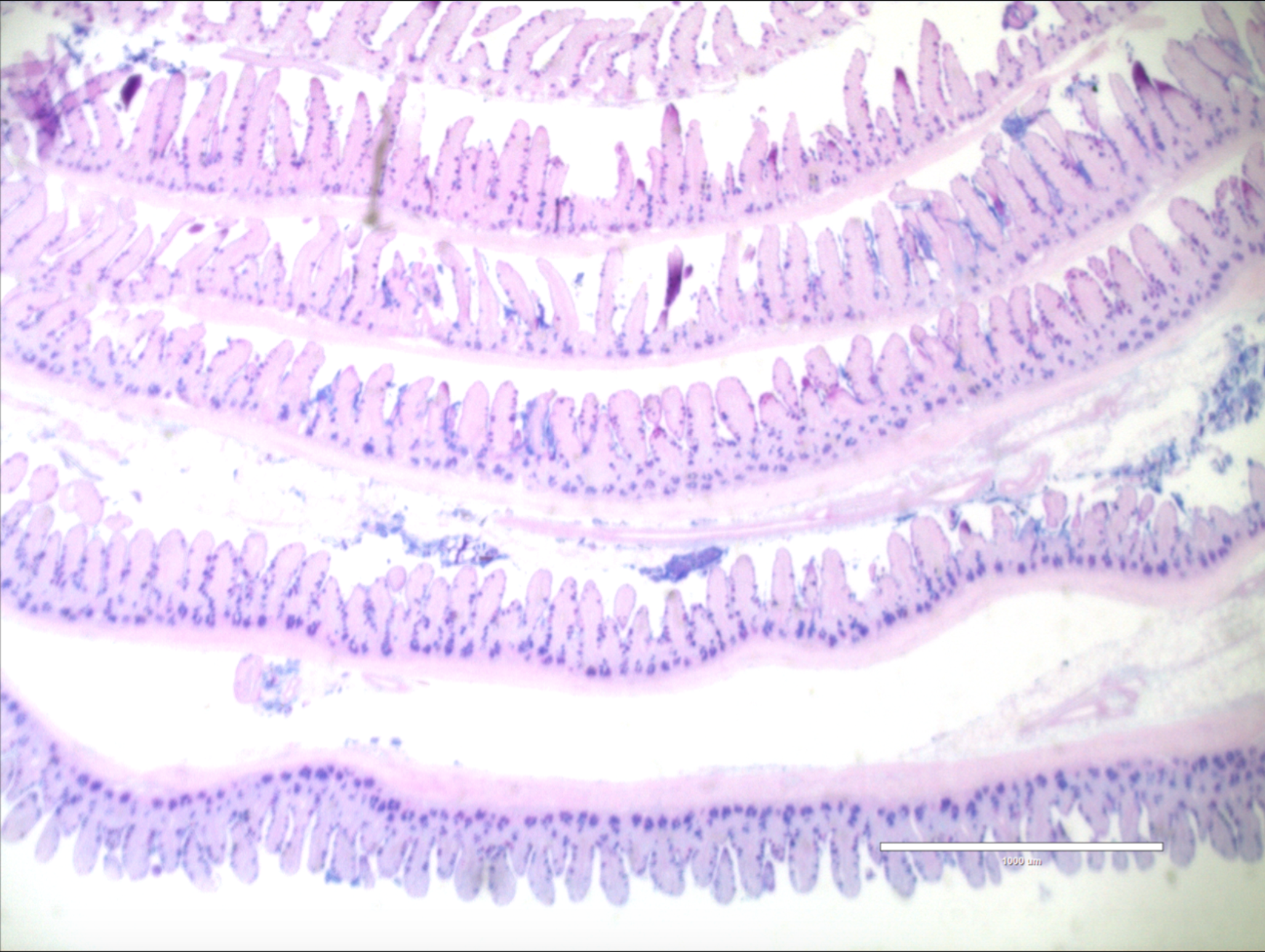
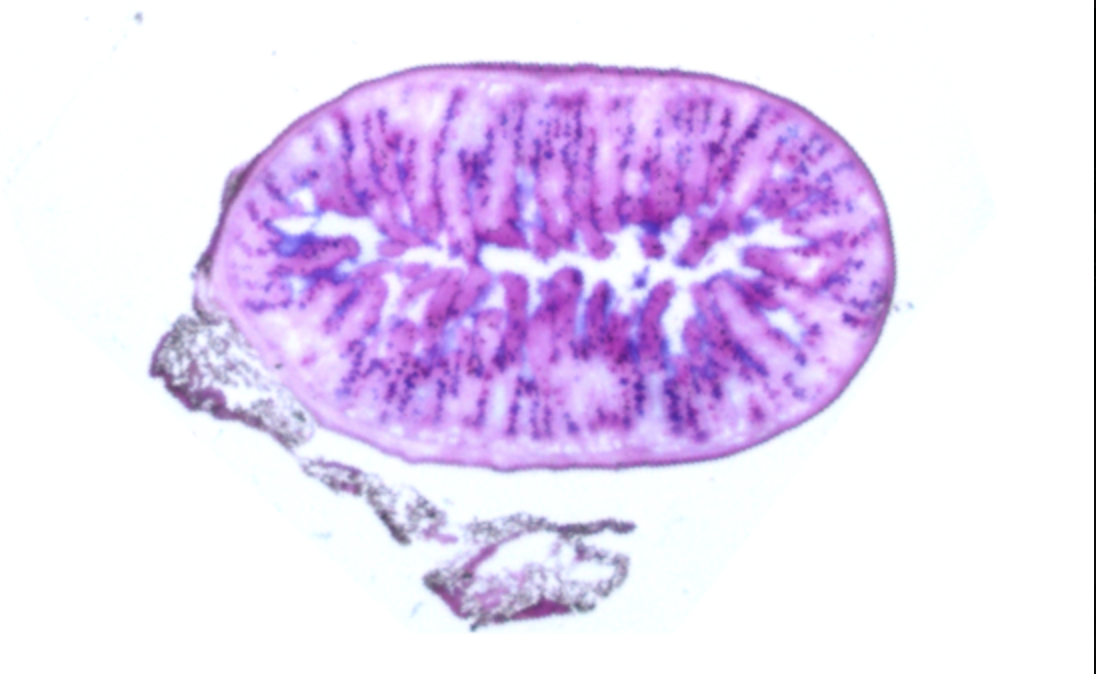
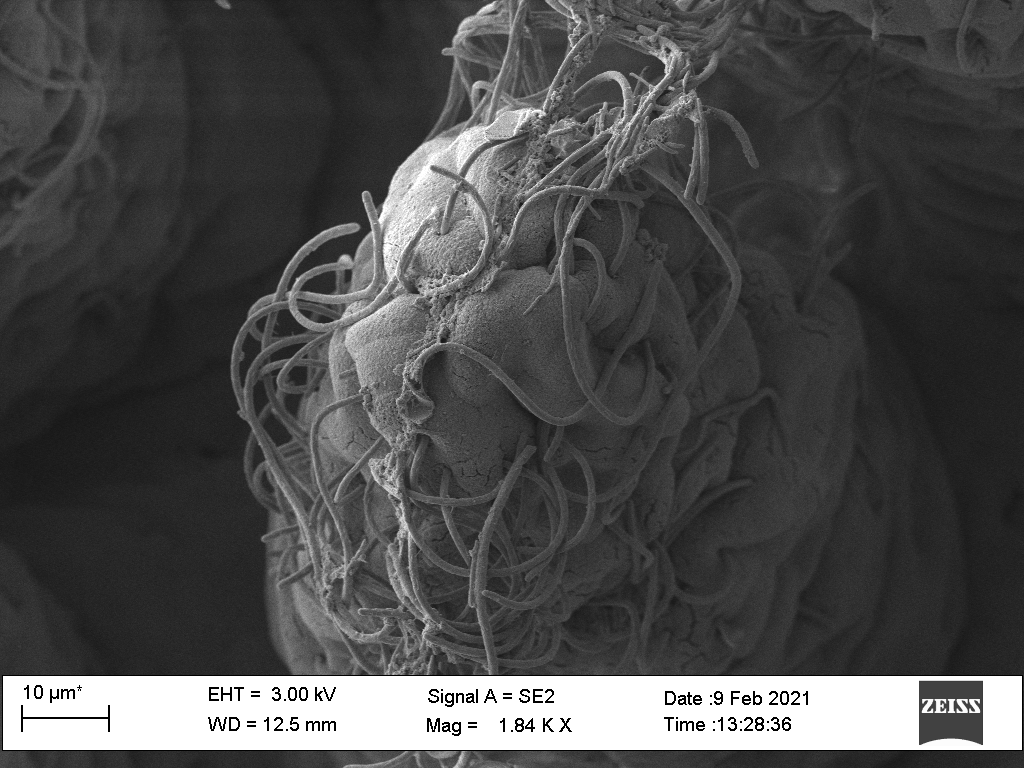
Project #2: Promoting myelin repair to increase neuroprotection.
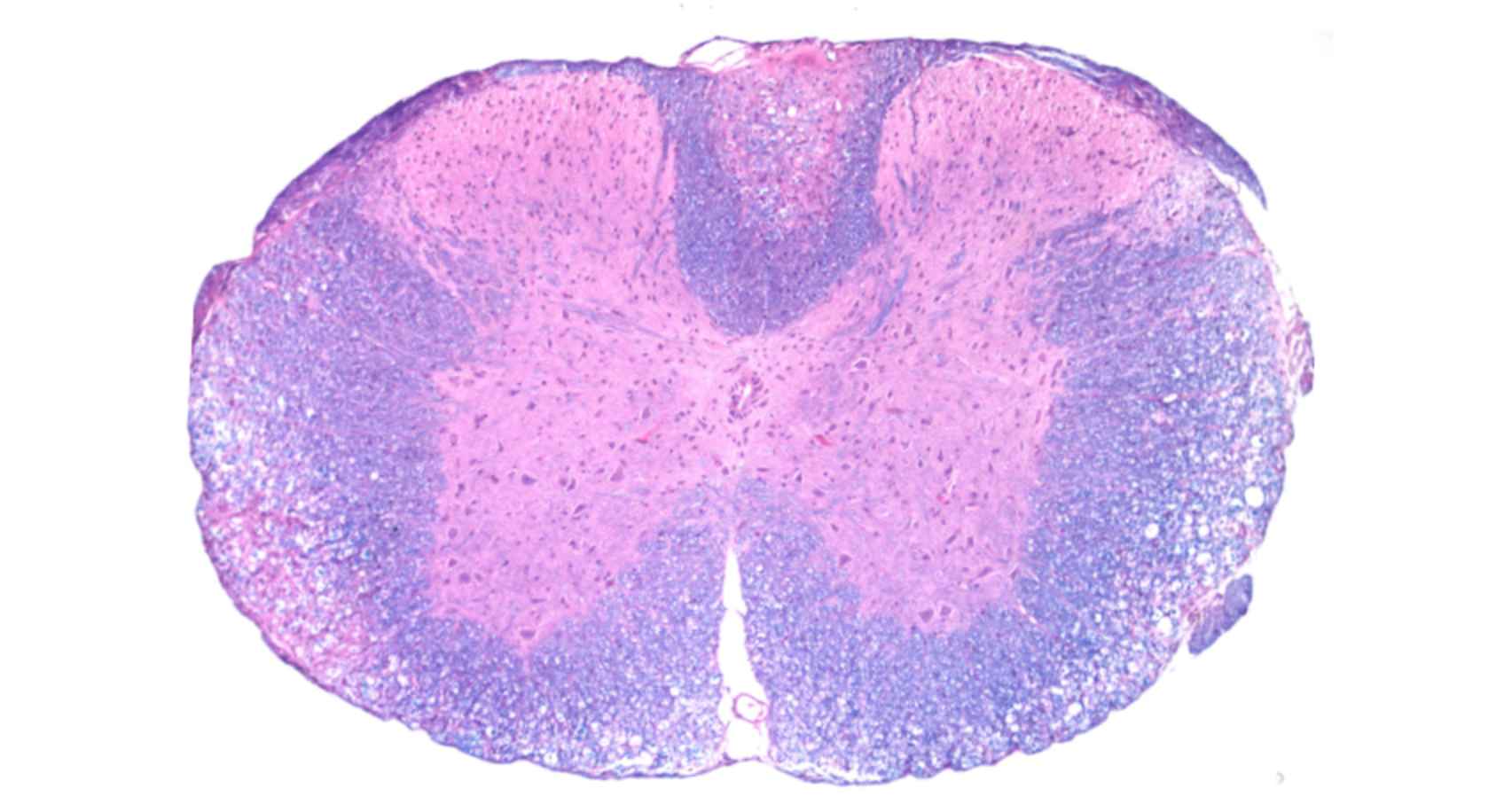
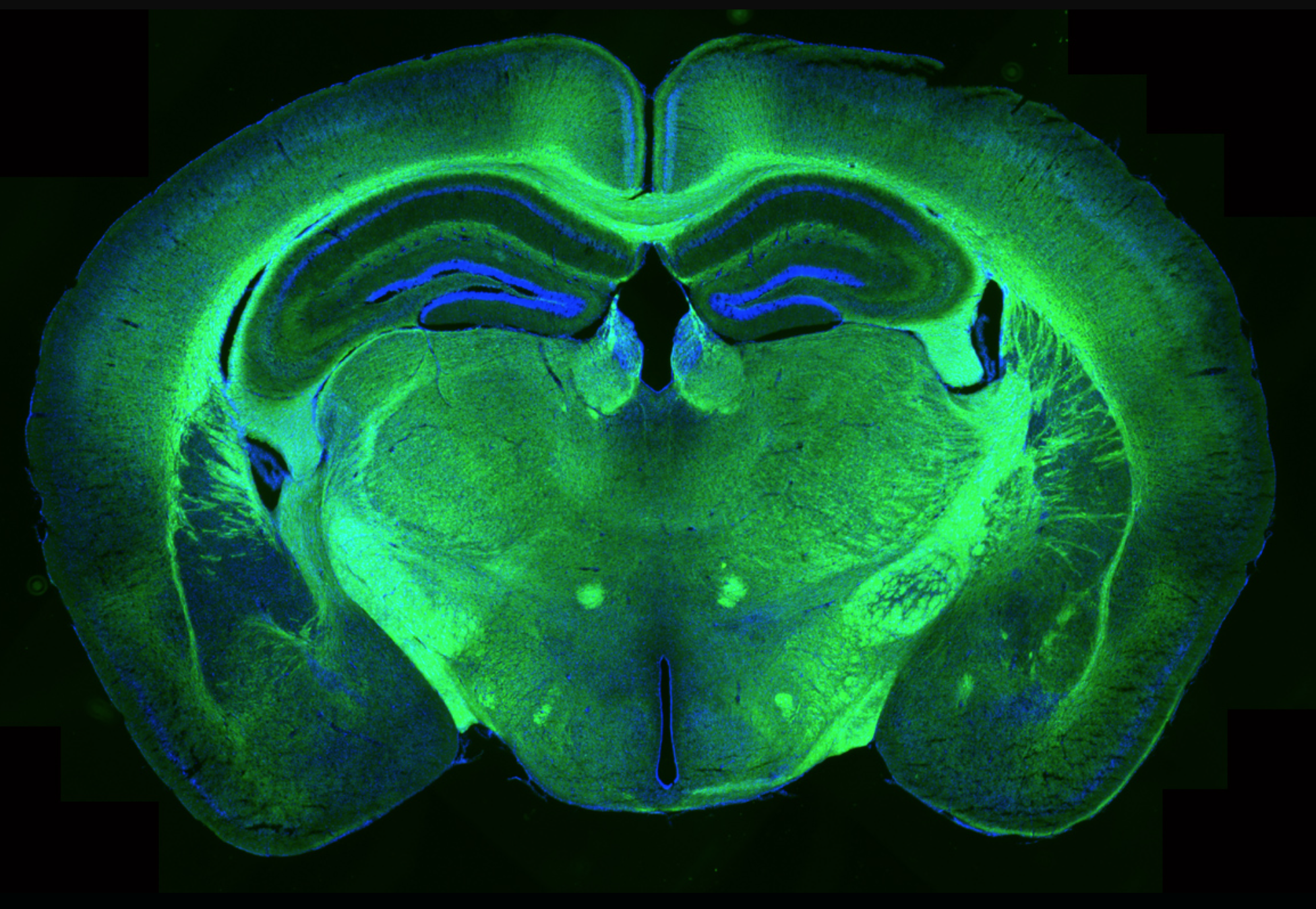
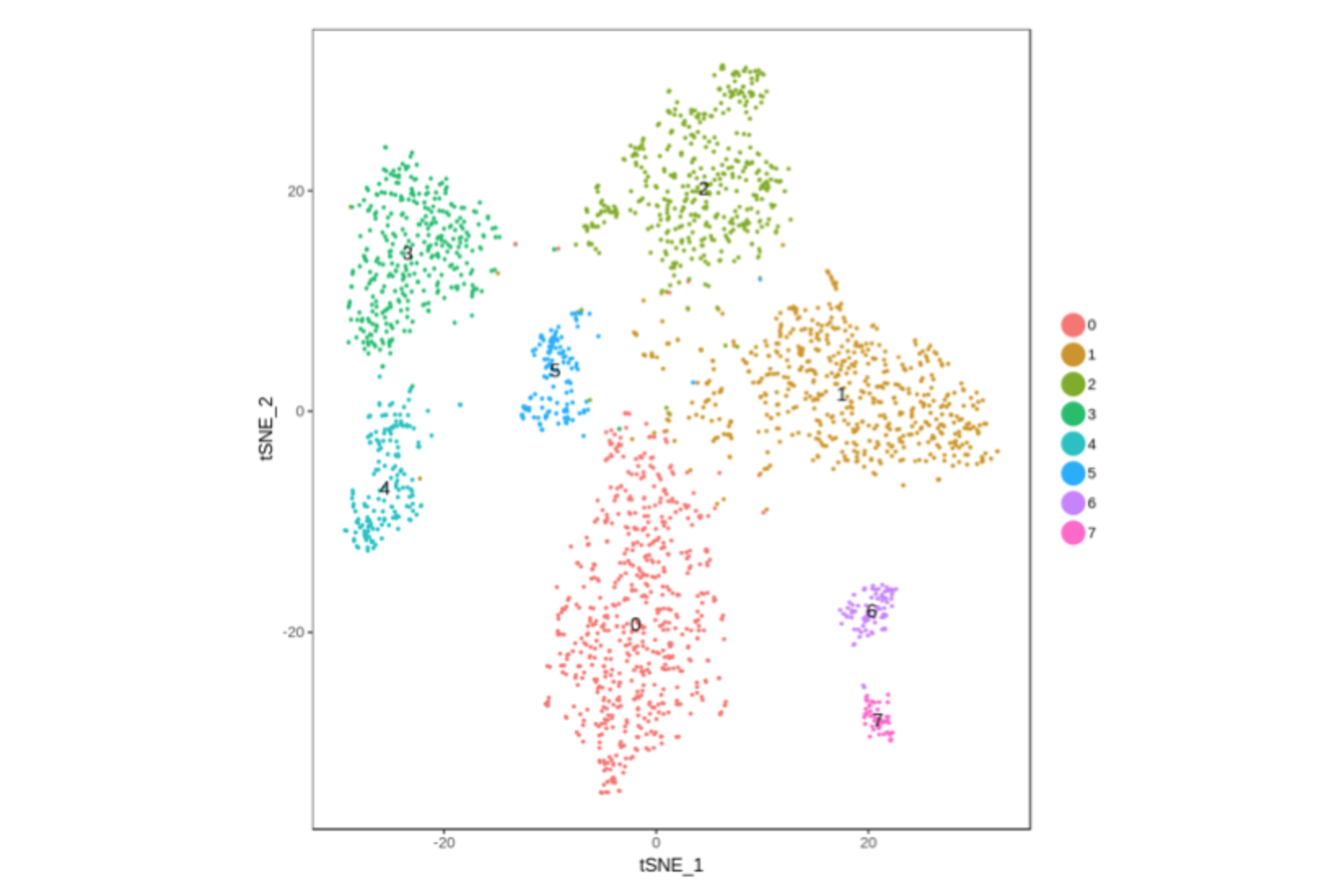
Chronic demyelination is a major reason for disease progression and increased disability in MS patients, as exposed neurons become prone to neurodegeneration. Unfortunately, currently approved therapies are only aimed at dampening the immune response and do not address the critical need for stimulating myelin repair during/following an MS attack. Understanding the mechanisms of remyelination is critical in preventing neuronal loss, and is paramount to improving the quality of life of MS patients. We are using a combination of bioinformatics and animal studies to further our understanding of remyelination with the hope to develop new therapeutic options.
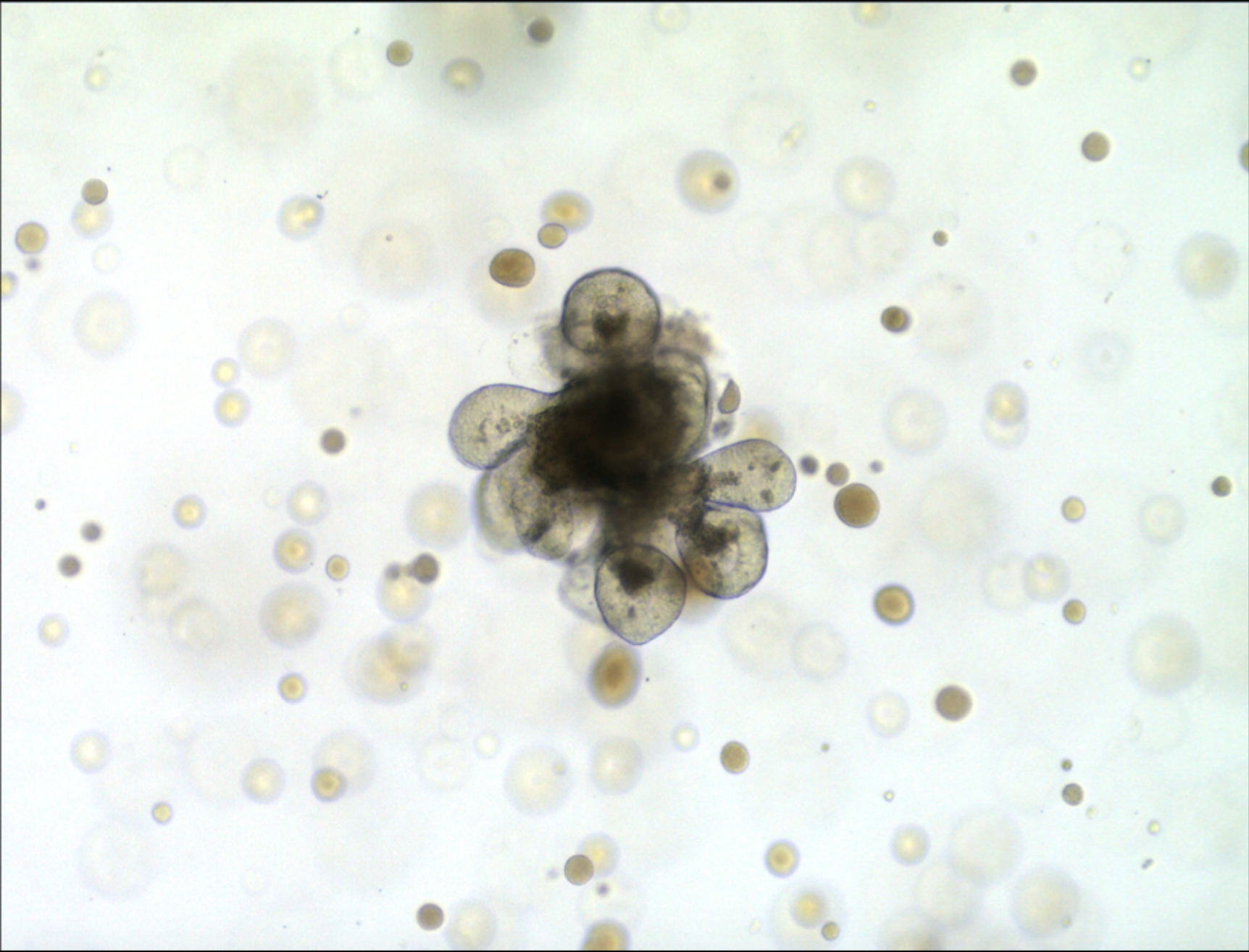
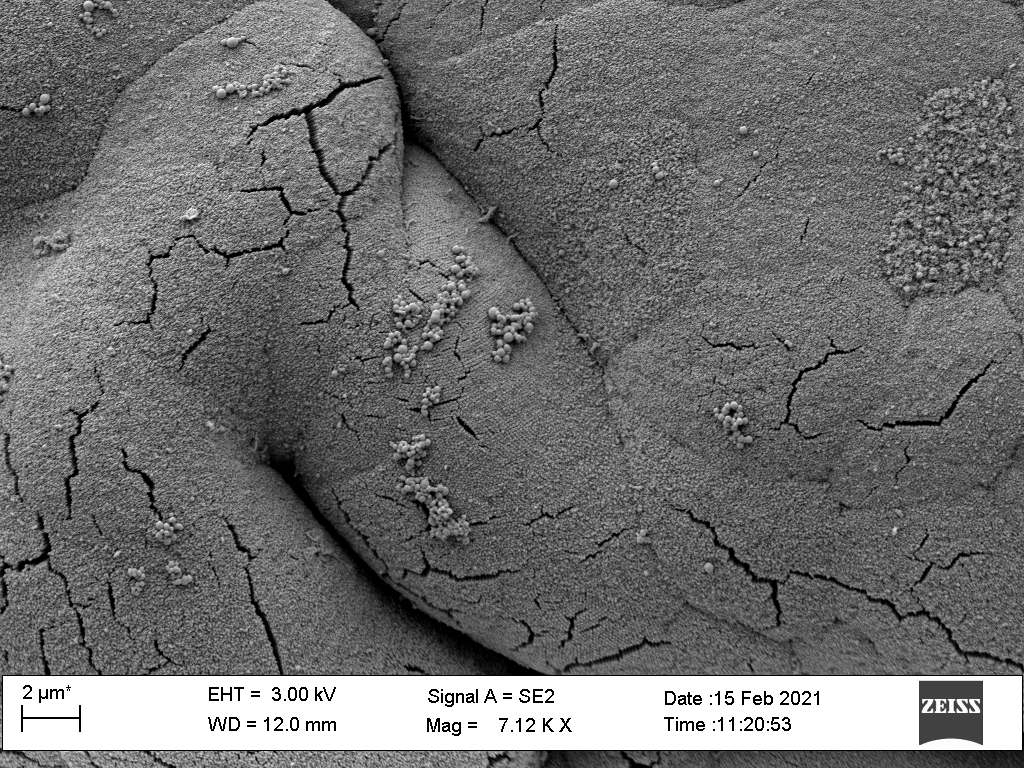
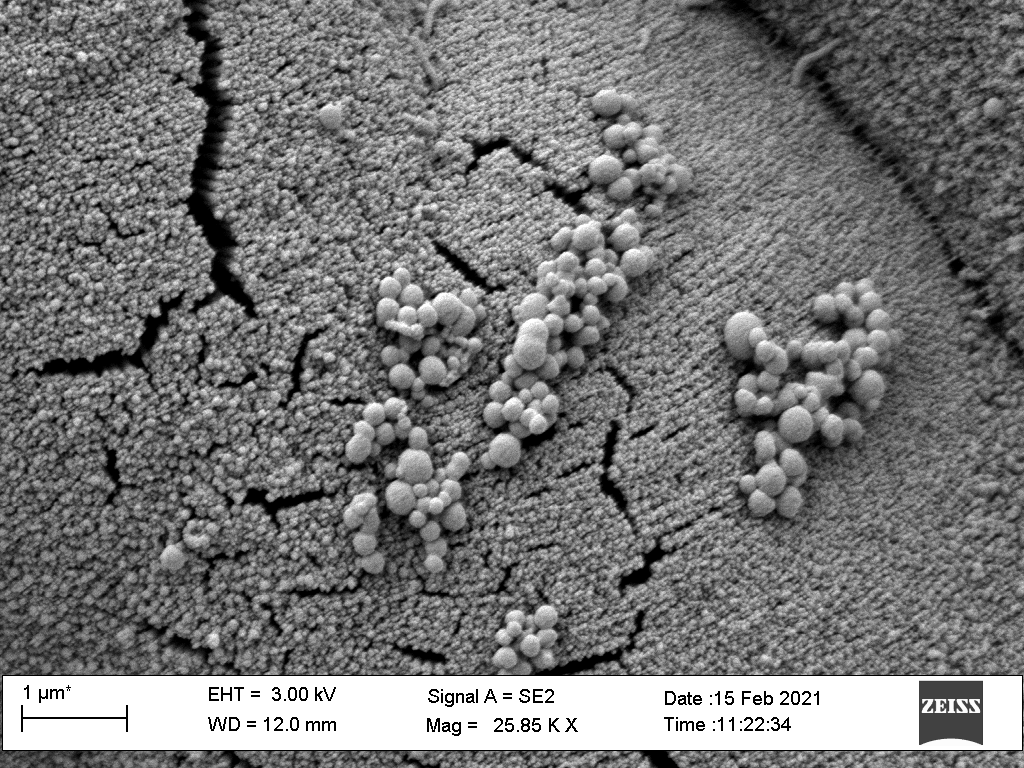
Project #3: understanding the links between the gut microbiome and mental health
Major depressive disorder is the most common group of symptoms observed in MS patients (20%) and affects 5% of the total US population. Current therapies for depression are marred with severe side effects and incomplete efficacy. We have demonstrated that the gut microbiome is an active participant in initiation and progression of depression. In particular, we have demonstrated that Lactobacillus species of bacteria influence the host biology and control the production of pro-depressive compounds. We are currently further exploring the connection between the microbiome and mental health.