We are a BIG deal.
We are a lab within the Center for Brain Immunology and Glia (BIG) at the University of Virginia’s Department of Neuroscience. The lab began with a primary interest in better understanding multiple sclerosis, which is an autoimmune disease that results in damage to the central nervous system, particularly to oligodendrocytes and neurons. Though we continue to look for means to therapeutically target multiple sclerosis, we have also begun to explore other disease models that touch on areas of neuroscience or immunology, as well as their intersection (neuroimmunology).
Project #1: Myelin Repair in Multiple Sclerosis
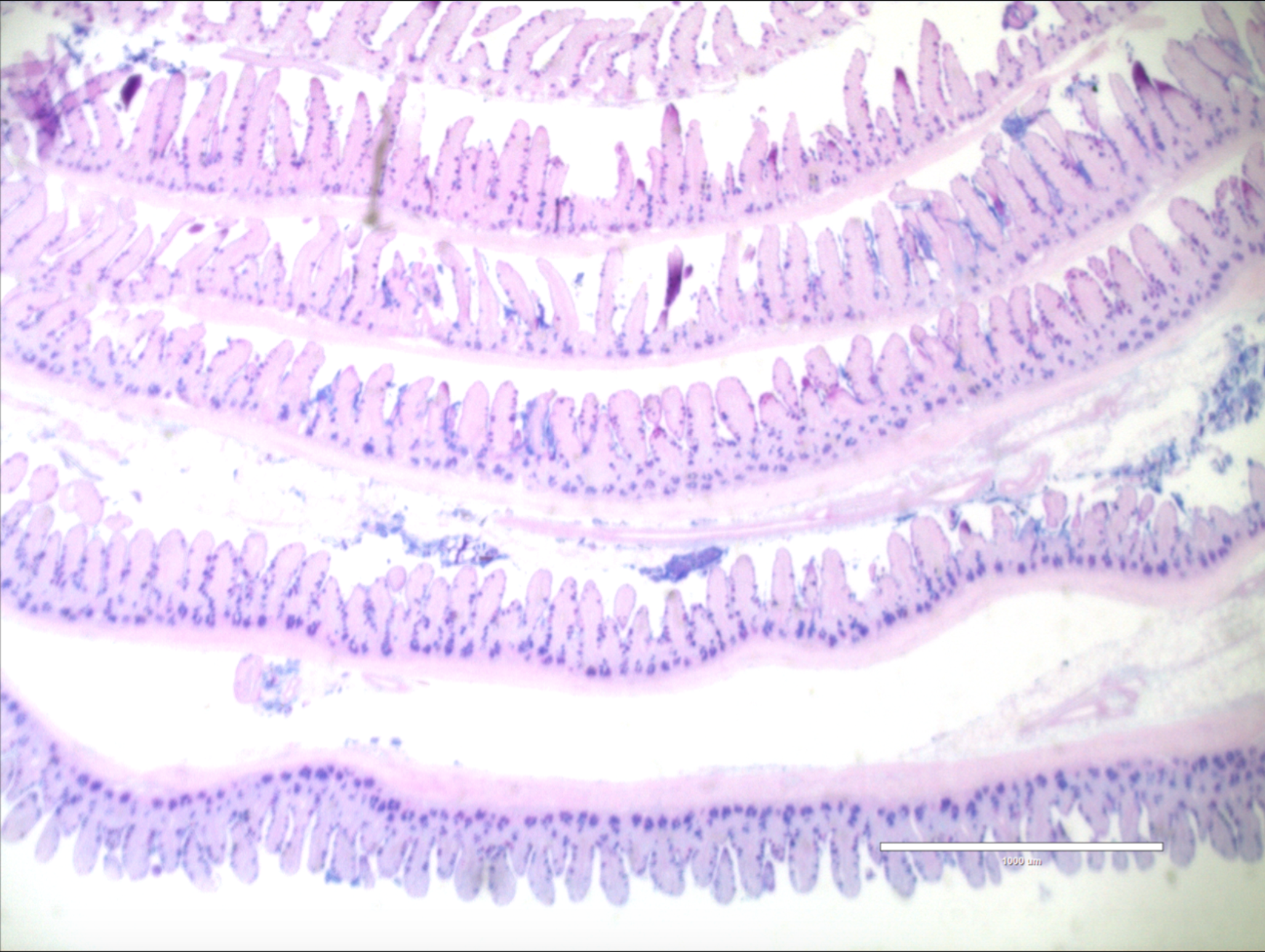
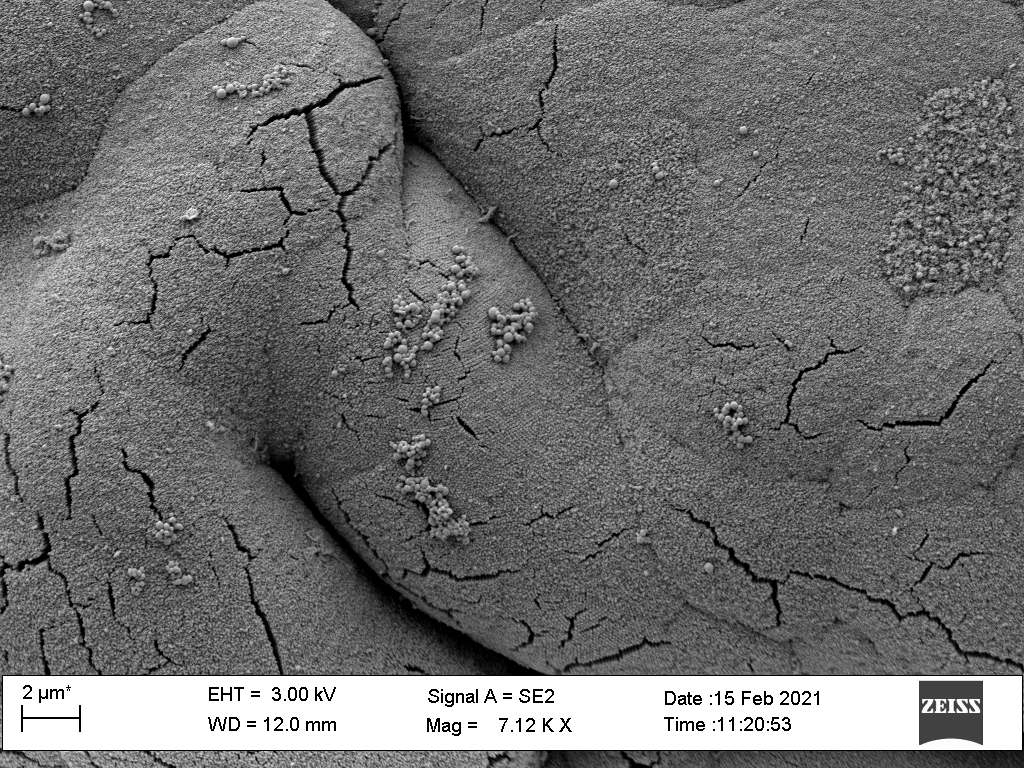
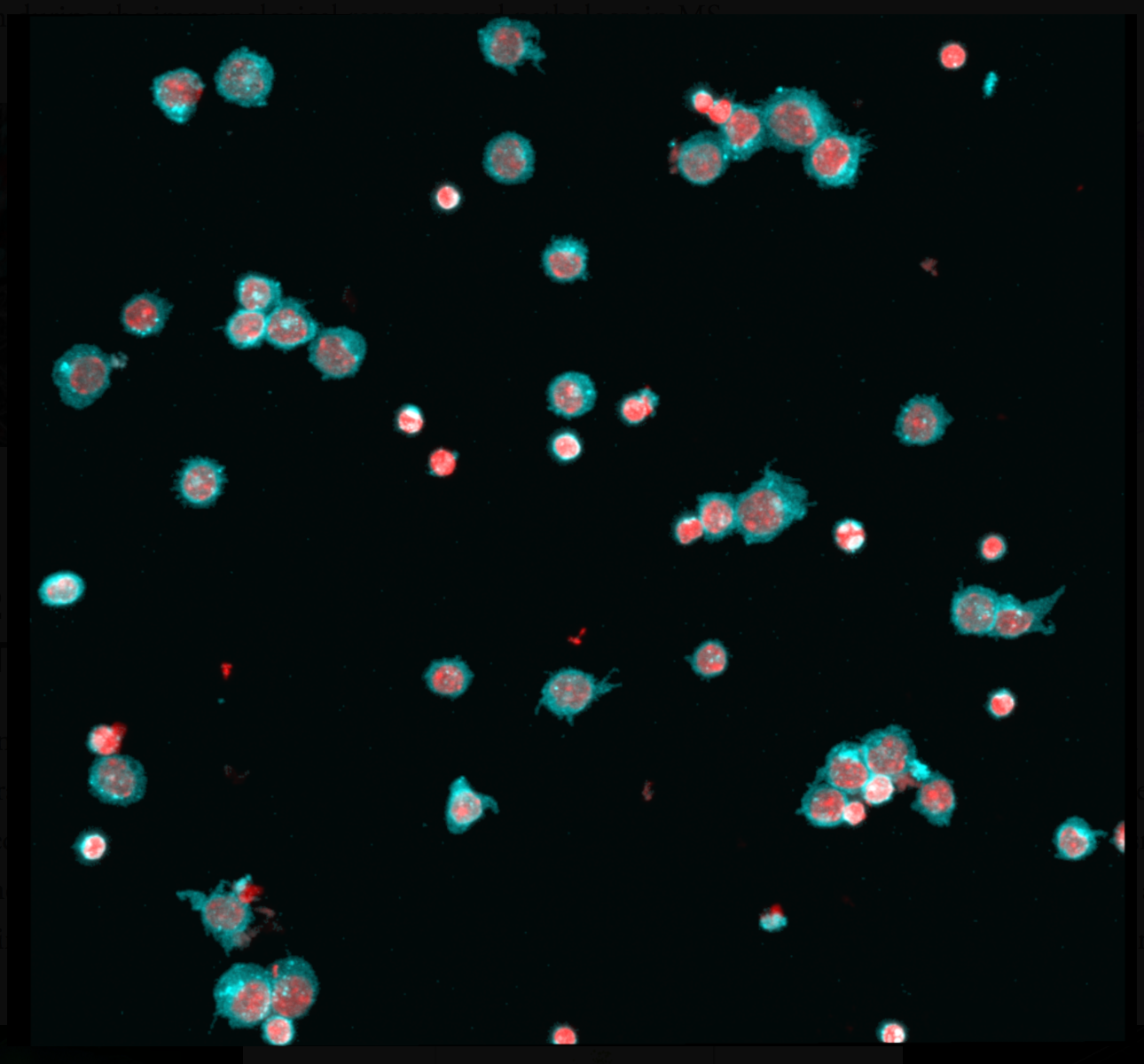
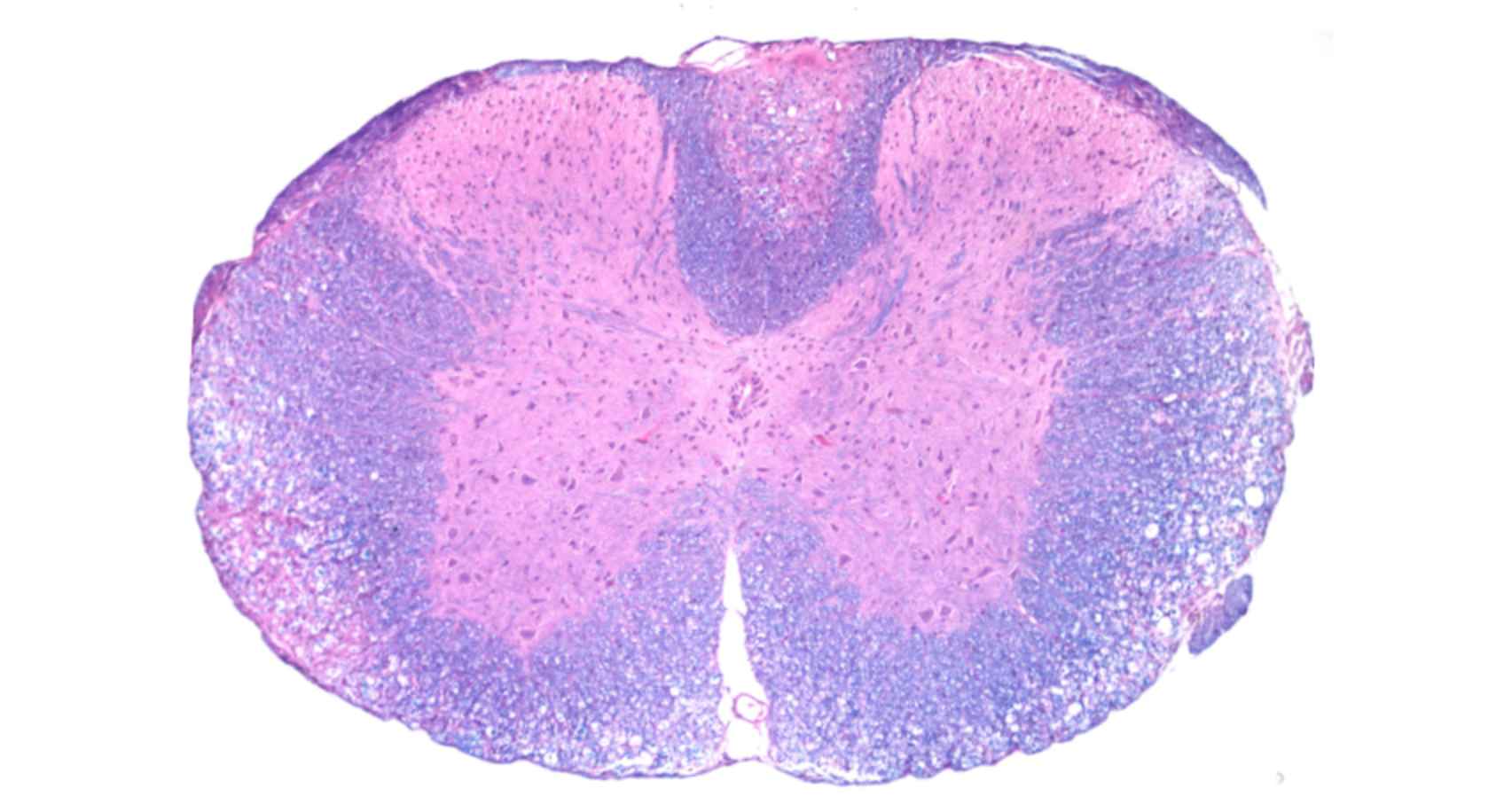
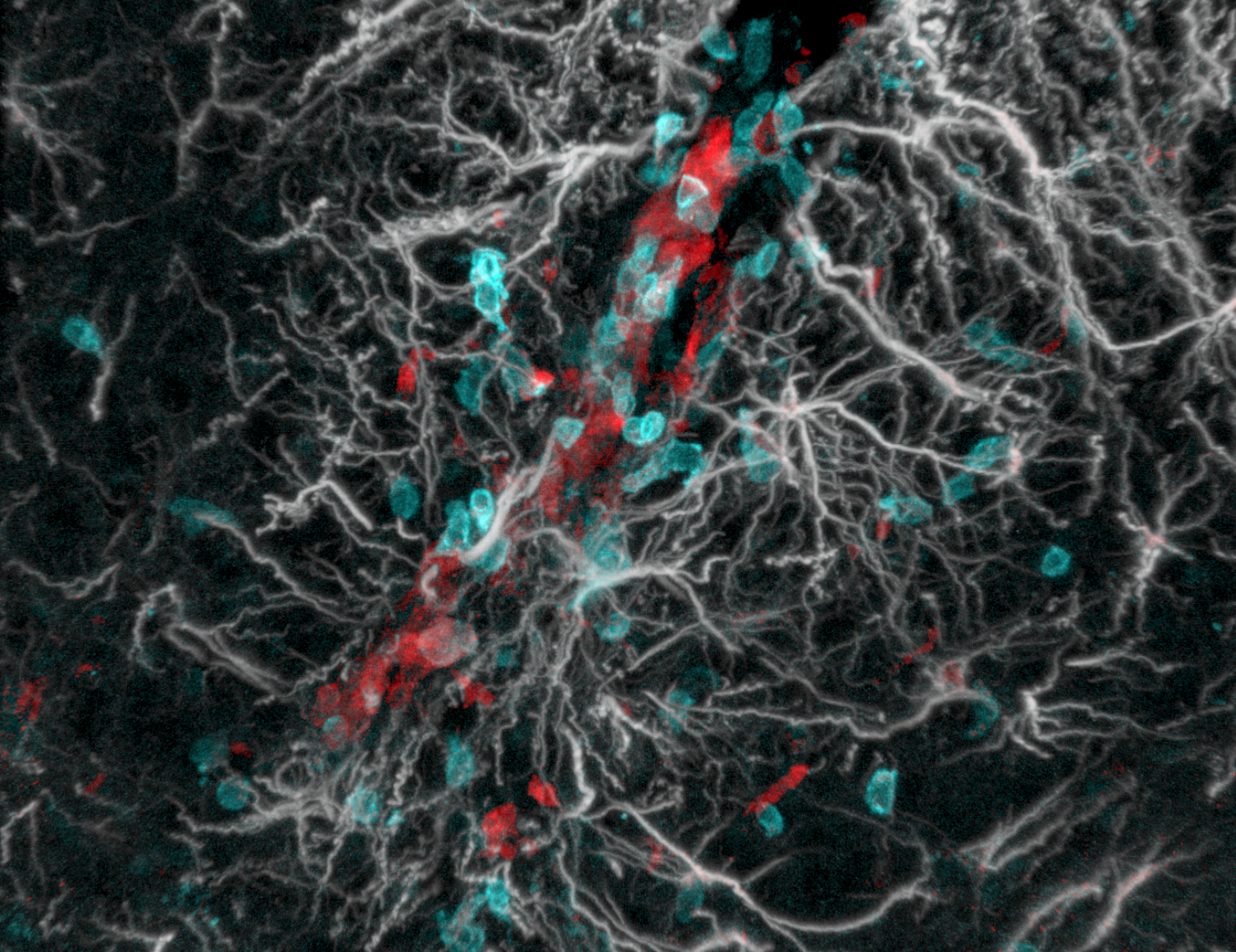
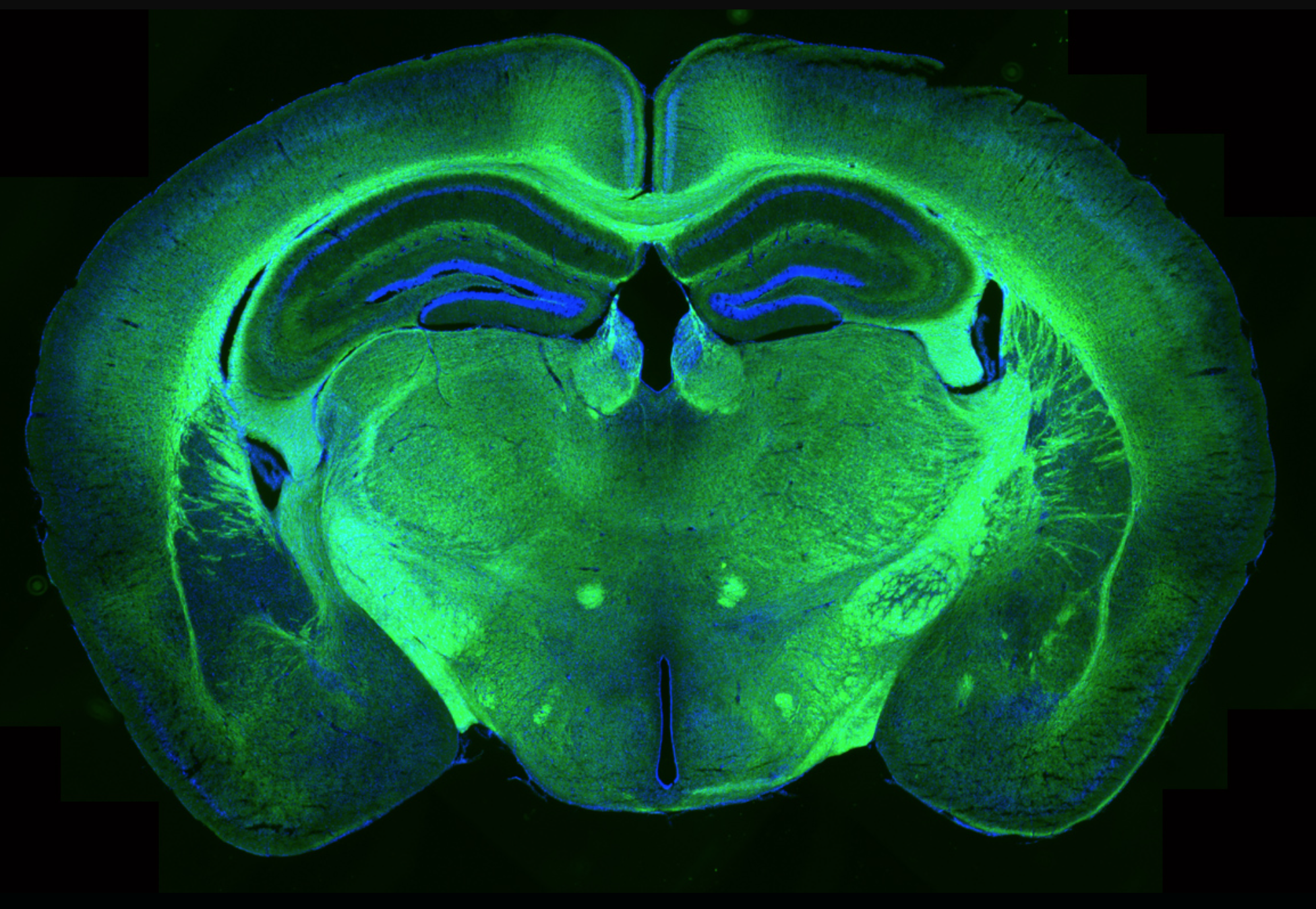
Chronic demyelination drives disease progression and disability in Multiple Sclerosis, as exposed neurons become prone to neurodegeneration. Understanding the mechanisms of remyelination is critical for the prevention of neuronal loss and is essential for improving the quality of life of Multiple Sclerosis patients. The brain contains a large population of oligodendrocyte progenitor cells that have the potential to differentiate into mature oligodendrocytes and remyelinate denuded axons, but this process is impaired in Multiple Sclerosis. Recent reports also suggest that oligodendrocyte progenitor cells can exert functions beyond myelination. Under pathological conditions, these cells are actively recruited to injury sites, where they orchestrate glial scar formation and contribute to the immune response. Our lab studies the biology of oligodendrocyte progenitor cells using animal models of Multiple Sclerosis to discover new treatments.
Project #2: myelin repair in ALZHEIMER’S DISEASE
In recent years, increasing amounts of data have pointed to myelin disruption as a significant pathological finding in Alzheimer’s Disease patients, and the concept that myelin disruption is a key event that contributes to and precedes cognitive decline in Alzheimer’s Disease is gaining increasing support. The hope is that finding therapeutic interventions to repair myelin could help protect neurons before irreversible neurodegeneration takes place. It remains unclear why oligodendrocyte progenitor cells, which can give rise to new myelin-producing oligodendrocytes throughout adulthood, fail to repair myelin in Alzheimer’s Disease. Even more unclear are the reasons why oligodendrocytes, the cells responsible for making myelin, malfunction in Alzheimer’s Disease patients. We are trying to address these important questions.
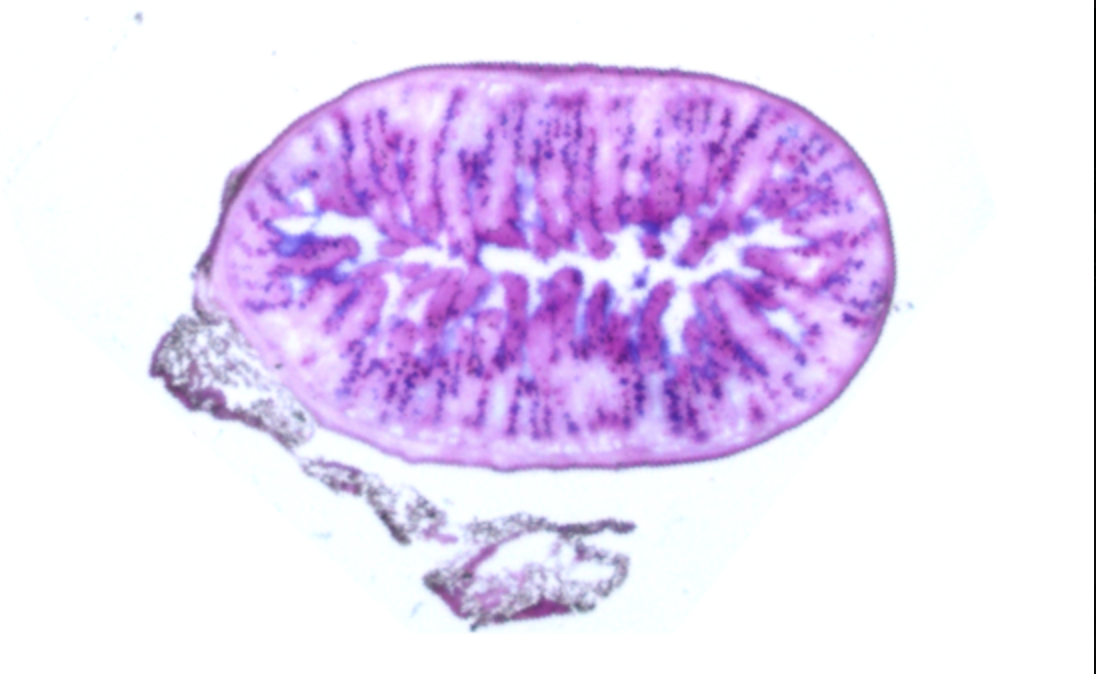
Project #3: The Role of the Gut-Brain Axis in Neurological Disorders
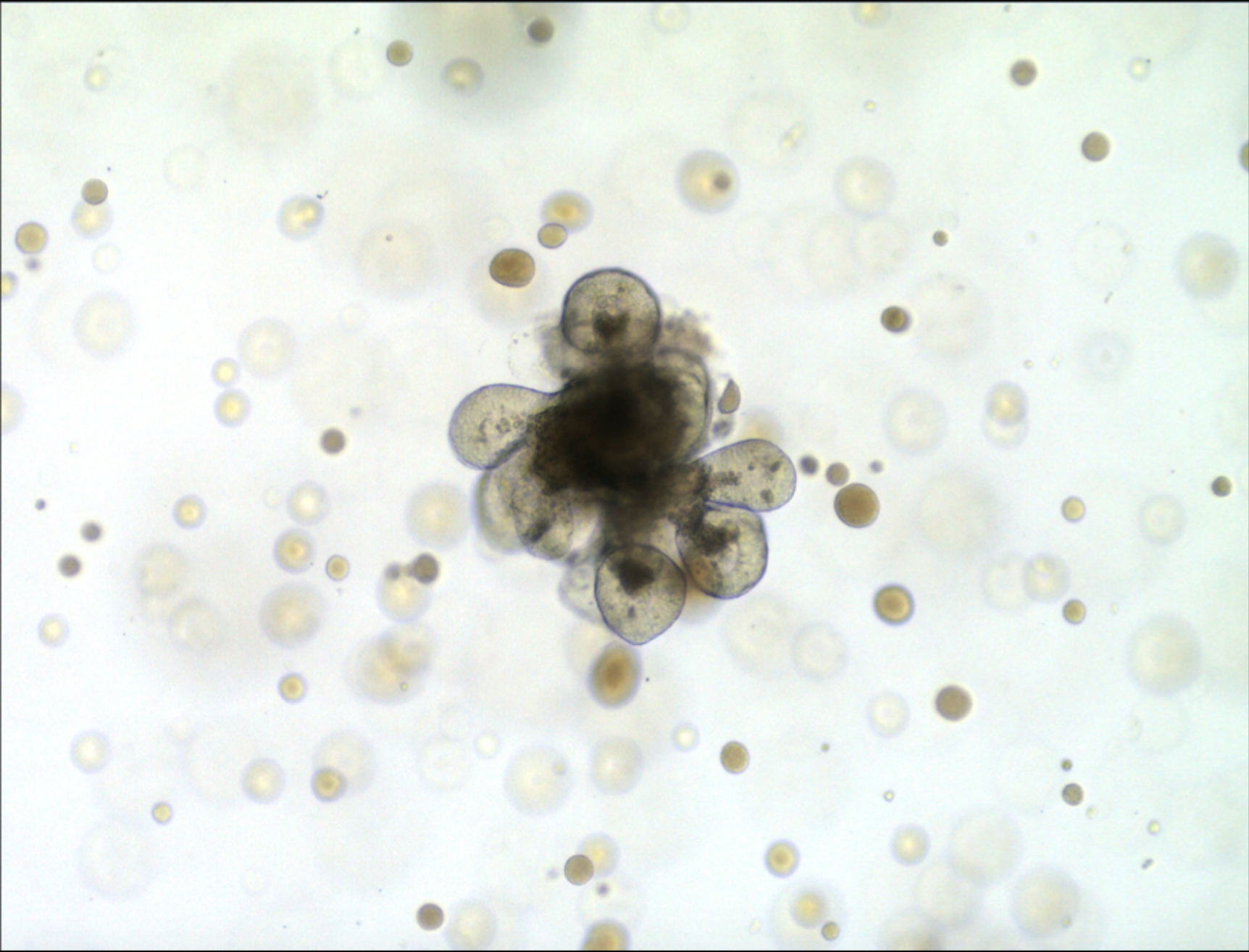
Gut microbiome dysbiosis is a hallmark of many human diseases and has been shown to actively contribute to disease pathology. Furthermore, therapies aimed at correcting dysbiosis and restoring the microbiome to homeostasis have been successful in experimental models of human disease and in dysbiotic patients. While it is widely accepted that gut-produced metabolites can influence the host in both homeostatic and pathological conditions, further research is needed to elucidate how relatively small quantities of these molecules can exert far-reaching effects, such as those observed by their action in the brain. Our lab is actively studying how gut-derived metabolites influence the progression of neurodegenerative conditions, such as Multiple Sclerosis and Alzheimer’s Disease.